For the first time, scientists have visualised an interaction between gluten and T-cells of the immune system, providing insight into how coeliac disease, which affects approximately one in 133 people, is triggered.
Published in Immunity, the discovery was led by Dr Hugh Reid and Professor Jamie Rossjohn of Monash University, Professor Frits Koning of the University of Leiden and Dr Bob Anderson of biotechnology company ImmusanT Inc, based in the US.
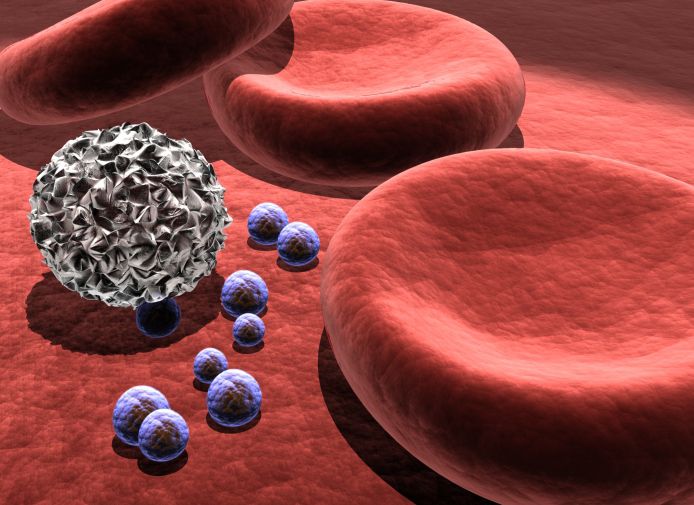
An increasingly-diagnosed chronic inflammatory disorder, coeliac disease affects the digestive process of the small intestine. When a person with coeliac disease consumes gluten, their immune system triggers T-cells to fight the offending proteins, damaging the small intestine and inhibiting the absorption of important nutrients into the body. There are currently no treatments available apart from a diet completely free of gluten.
The researchers used the Australian Synchrotron to visually determine how T-cells of the immune system interact with gluten, a protein found in wheat, rye and barley, which causes coeliac disease. The discovery will boost attempts to produce a treatment allowing sufferers to resume a normal diet.
About half the population is genetically susceptible to coeliac disease because they carry the immune response genes HLA-DQ2 or HLA-DQ8. At least one in 20 people who carry HLA-DQ2 and about one in 150 who have HLA-DQ8 develop coeliac disease, but people with other versions of the HLA-DQ genes are protected.
This has led researchers to question how the immune system senses gluten.
Dr Reid, a senior research fellow at Monash said the discovery was an important breakthrough for coeliac disease and autoimmune disease.
“This is the first time that the intricacies of the interaction between gluten and two proteins that initiate immune responses have been visualised at a sub-molecular level,” Dr Reid said.
This insight into a central event in coeliac disease will assist ImmusanT to develop a blood test and a therapeutic vaccine, Nexvax2®, for patients with coeliac disease who carry the gene HLA-DQ2. It is intended to restore immune tolerance to gluten and allow patients to return to again include gluten in their diet.
Future studies will investigate whether T-cell activation by gluten in patients with HLA-DQ2 follows similar principles as observed in this study that focused on HLA-DQ8-mediated coeliac disease.
Chief Scientific Officer at ImmusanT, Dr Bob Anderson said the research presented a unique opportunity.
“Because we now know the gluten peptides responsible for coeliac disease, we can interrogate the molecular events leading to a self-destructive immune response,” Dr Anderson said.
Source: Monash University